HIV: Adolescents and young adults, a particularly high-risk population
From 2012 to 2016, Médecins Sans Frontières (MSF), in collaboration with Ministries of Health, conducted 5 large-scale population-based HIV surveys in 4 African countries with high HIV prevalence and long-standing HIV programmes: Ndhiwa in Kenya, KwaZulu-Natal in South Africa, Chiradzulu and Nsanje in Malawi and Gutu in Zimbabwe. Each randomly selected participant aged between 15 and 59 in the region concerned was interviewed and given a rapid HIV test. If the test was positive, further blood tests were carried out to measure CD4 levels and viral load in the blood, a key indicator of therapeutic success. A total of 28,813 people were included.
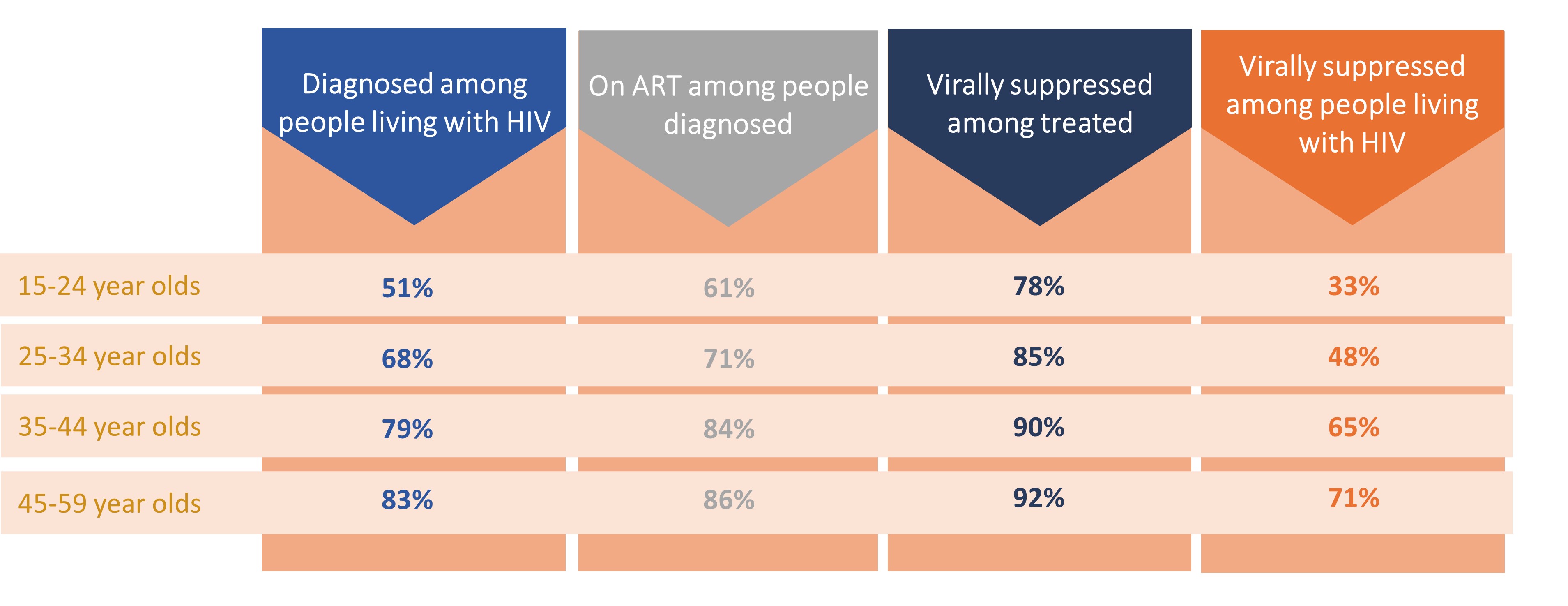
The first parts of the analyses made it possible to assess where these populations were in relation to the UNAIDS objectives, which were 90-90-90 for the period under consideration: 90% of people living with HIV who know their HIV status, 90% of these people who have access to antiretroviral treatment (ARV), and 90% of people on ARV who have their viral load suppressed. The current targets are 95-95-95. All ages combined in the cohorts in these 5 contexts in Eastern and Southern Africa, 73% of people living with HIV were diagnosed, 79% of those diagnosed were on ARV treatment and 88% of those on ARV had their viral load permanently suppressed.
"If we look at the general population, none of the UNAIDS indicators were met in 2016, but we wanted to go a step further and assess coverage of HIV diagnosis and treatment by age group and sex," explains Jihane Ben Farhat, epidemiologist at Epicentre and co-leader of the study. And the results highlight major disparities according to age.
Adolescents and young adults: under-diagnosed and less often treated
The proportion of undiagnosed people is increasing among the youngest age groups: only 1 in 2 teenagers and young adults living with HIV is diagnosed, compared with more than 8 in 10 in the 45-54 age group. And only 60% of diagnosed adolescents and young adults are on antiretroviral treatment. Treatment coverage also appears to be poorer, with fewer than 78% of 15–25-year-olds on treatment having their viral load suppressed (below 1,000 copies/mL), compared with 92% of 45-59-year-olds.
"While the UNAIDS 90-90-90 targets have been or are about to be achieved in the over-35s, this is far from being the case in the younger population," notes Helena Huerga, epidemiologist at Epicentre and co-responsible for the study.
Overall, only 1 in 3 adolescents or young adults living with HIV has a suppressed viral load (less than 1,000 copies/mL). These results call into question the relevance and adequacy of all stages of care, from screening to proper follow-up, including initiation of treatment and access to the various biological tests, for this age group.
An effect accentuated in teenage girls and young women
Taking all ages together, although men are more often under-diagnosed, there is no difference between the two genders in terms of treatment coverage and viral load suppression. If we focus on the 15-24 age group, 42% of teenage girls and young women and 23% of teenage boys and young men diagnosed were not on treatment. And 1 in 4 women aged between 15 and 24 and almost 1 in 10 men had a viral load of more than 1000 copies/mL, despite being on treatment.
"One of today's challenges is to improve treatment initiation in these populations, followed by good compliance, which is necessary to achieve an undetectable viral load," concludes Jihane Ben-Farhat.
Priority to teenagers and young adults
Factors explaining under-diagnosis include stigma, but also lower use of health centres by men and the impact in terms of acceptance of diagnosis and treatment. Some young adults prefer to self-diagnose, which proves that age-appropriate solutions exist and can be implemented. But this requires healthcare systems to make specific provision for adolescents and young adults, which is hardly the case in most countries. After having benefited from very close monitoring in pediatric services, young people most often switch without any transition or support to services dedicated to adults. As a result, a number of them leave care. The implementation and evaluation of dedicated interventions adapted to this age group, such as the "teens clubs" deployed by MSF in Malawi, appear to be able to limit this break with care and improve diagnosis, as well as engagement and retention in HIV treatment and care.
These strategies must also incorporate social media or young peers, which are highly valued by this population, and prevention initiatives to reduce the number of new infections. The aim is to provide young people with a range of services and information tailored to their needs, in places that are dedicated, welcoming, confidential, easy to access and affordable, where they can talk and exchange ideas, without paternalism.











