A 2-in-1 to screen cervical cancer in Malawi
What is the PAVE study?
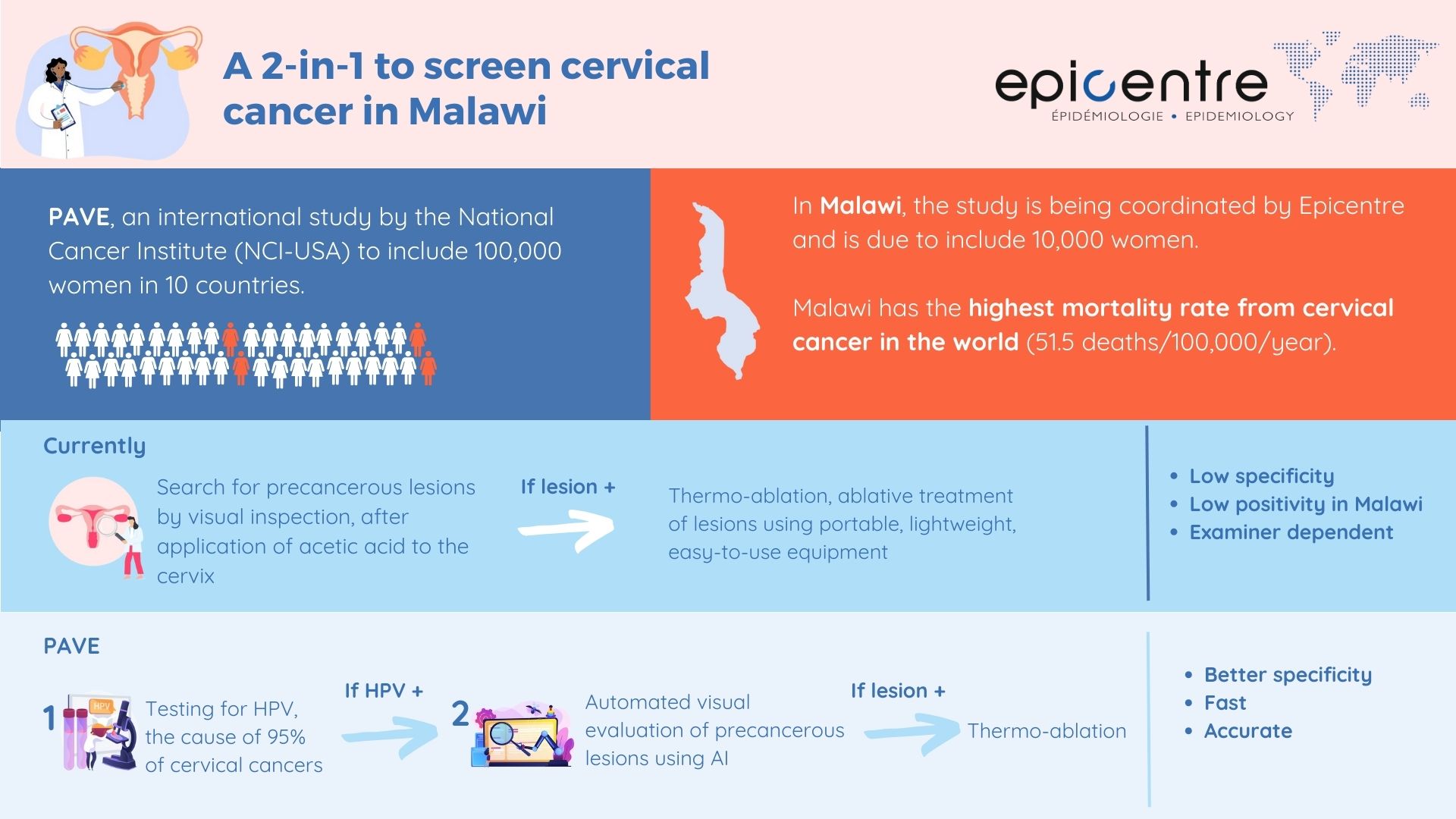
Amna Haider: The aim of the PAVE study is to evaluate and optimize a new screening-triage-treatment algorithm for cervical cancer. Once detected at an advanced stage, the chances of curing this cancer - the 4th most common among women worldwide - are low. The challenge is therefore to diagnose it as early as possible, ideally at the precancerous lesion stage. In 95% of cases, this cancer develops following infection with a papillomavirus (HPV) transmitted during sexual intercourse. This virus inserts itself into the genetic material of cells and triggers their transformation into cancerous cells. At the start of this process, a precancerous lesion is formed, which can be seen by simple visual inspection after the application of acetic acid to the cervix and is easily treated.
The strategy proposed by the US National Cancer Institute as part of the PAVE study initially involves detection combined with HPV genotyping and then, in women with high-risk HPV, automated visual evaluation (EVA) using an algorithm that recognizes precancerous lesions on digital images of the cervix. The algorithm was trained on a sample of representative images of cervical precancers and healthy tissue to identify these lesions. In a previous study, it was shown to outperform other screening tests, in particular screening by visual inspection of the cervix by a health professional. It now needs to be validated on a larger scale in low- and middle-income countries. This new triage strategy is proving to be relatively inexpensive, rapid, accurate and reproducible. In the PAVE study, the reference test is histopathology of tissue samples taken from all participants with a positive HPV screening test.
The NCI-led consortium includes 10 study sites (Nigeria, El Salvador, Tanzania, Malawi, Eswatini, Cambodia, Honduras and the Dominican Republic and 2 in Brazil) and will involve 100,000 women. With the support of the MSF Foundation, I am coordinating the Malawi site.
What are the special features of this site?
Amna Haider: Every year in Malawi, more than 4,000 women are diagnosed with cervical cancer, and almost 3,000 women die from it. Malawi has the highest mortality rate from cervical cancer in the world (51.5 deaths/100,000/year). This rate is twice that observed elsewhere in East Africa and seven times higher than the global rate. MSF has been involved in cervical cancer screening and treatment for several years, in collaboration with the Malawian Ministry of Health at 10 health centers and their catchment areas in Blantyre and Chiradzulu districts in Southern Malawi.
Despite existing campaigns, cervical cancer screening coverage is still well below the national target of 80% of women screened by visual inspection at least once. A survey conducted by Epicentre in 2019 showed that only 40% of women had been screened in Blantyre, and even fewer in the rural area of Chiradzulu (1). Although it is not the only weapon in the fight against cervical cancer, screening, as a complement to prevention, has an essential role to play in reducing mortality by early detection from this cancer in Malawi.
Following approval from the local ethics committee, the PAVE study began in Malawi in September 2023. Initially, we are going to 'train' the algorithm to recognize precancerous lesions, as there may be differences depending on the population, but also on the type of HPV causing the lesions. Ultimately, as part of a complementary study, we plan to investigate the carcinogenic potential of HPV 35 in the context of Malawi. While the forms commonly responsible for precancerous lesions are HPV 16 and 18, there are almost 200 types of HPV worldwide, and one study has shown that HPV 35 is very common in the Malawian population (2).
Our next objective is to offer this screening protocol to 10,000 Malawian women. Women identified as having a precancerous lesion or high-risk HPV virus infection will be treated by thermo-ablation. The study also includes a two-year follow-up to assess the cure rate of women who have undergone thermo-ablation at 1 and 2 years. Another feature of the Malawi study is to observe how precancerous lesions develop in women living with HIV compared with those without. Women living with HIV are six times more likely to develop cervical cancer than other women.
What are the expected benefits?
Amna Haider: MSF's precancer screening programme is currently based mainly on visual inspection. However, the positivity rate appears to be extremely low in the Blantyre and Chiradzulu sites compared with what can be observed in fairly similar sites, which raises the question of the quality control of screening activities and the reliability of visual identification of precancerous lesions, even by experienced nurses or doctors. With this study, we hope to improve screening of Malawian women and thus contribute to reducing cervical cancer mortality.
In addition, this study will enable us to upscale current screening strategy of visual inspection to HPV testing. The new assay used for testing for HPV viruses is faster and less expensive than the GeneXpert test currently used in limited facilities in Malawi, which should speed up the number of tests carried out.
If this screening method proves effective, it could also be offered to a larger number of women in Malawi and throughout the world. Given that over 90 per cent of deaths from cervical cancer occur in low- and middle-income countries, this is a real hope for reducing the incidence of this cancer, which if not detected early requires treatment with radiotherapy or chemotherapy, which is often unthinkable in these contexts.









