Covid-19 pandemic: a halt in the fight against HIV?
At the beginning of 2021, Malawi and Uganda appeared to be on track to meet the UNAIDS 90-90-90 targets, i.e., 90% of people living with HIV know their status, 90% have access to antiretroviral (ARV) treatment, and 90% of those on ARVs have sustained viral load suppression. The achievement of these goals is based on a constant effort and regular monitoring of people living with HIV. This also masks disparities by age group: while the targets were almost met for the general population living with HIV, this is far from being the case for younger people (1). Both countries were preparing to move to the 95-95-95 target, which offers the prospect of an end to the epidemic, when the Covid-19 pandemic began. In response, Uganda opted for a long lockdown, one of the strictest in the entire African continent (2). Malawi did not experience such restrictive measures, but experienced a sharp increase in the cost of living.
COVID19 pandemic and its deleterious effects in the fight against HIV
The measures implemented in both countries have led to disruptions in health care systems. To understand the impact, Epicentre conducted a study in the two sites where MSF supports ministries of health in monitoring and caring for people living with HIV, in Arua, Uganda and Chiradzulu, Malawi.
"At the beginning of the pandemic, initiations of antiretroviral (ARV) treatment dropped by 50% in Arua and by 34% in Chiradzulu. Clinical visits decreased by 68% in Arua and 60% in Chiradzulu," says Jihane Ben Ben-Farhat, an epidemiologist at Epicentre. We also saw in Uganda a 15% decrease in the number of adults followed up between Q1 2020 and Q1 2021, and 17% of children and adolescents."
In Malawi, this decrease is smaller [10% and 12%, respectively] and is only seen for those on 1st or 2nd line treatment, not those on 3rd line.
Among the reasons cited by people who no longer went to clinics for ARV refills or counseling was fear of contracting COVID-19. Health facilities were generally considered "crowded" with patients waiting next to each other. For example, a 44-year-old man in Chiradzulu said, "I was afraid because it was so crowded [at the clinic]. People were crowding in and we were coming home late, even though we came early. [...] Corona can be contracted in crowded places."
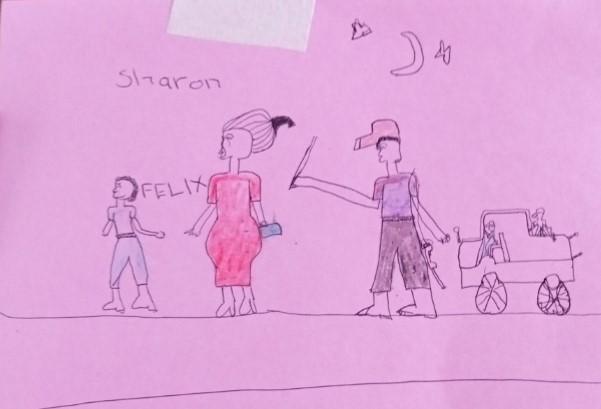
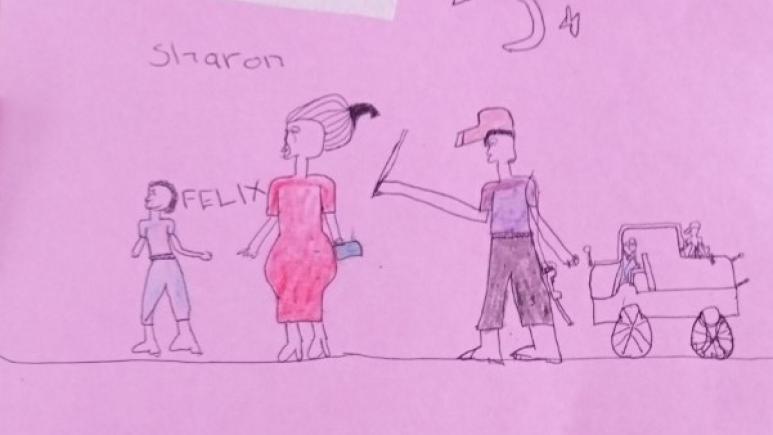
In addition, it was difficult to get to the health center because of transportation restrictions. The testimonies collected also mention the violence of the authorities in Uganda, as illustrated by this drawing made during a workshop set up by MSF to stimulate discussion among adolescent girls living with HIV about their day in COVID-19. Through it, Sharon explains that she did not go to the hospital because of the soldiers who beat people in the street. [...] She and her brother Felix were pressed for time - it was past curfew. The soldiers started hitting them. They had to make up a lie to get the soldiers to leave them.
Adapting the follow-up and management
Already widely practiced for several years, adapting not only monitoring but also ARV delivery models to people and their lifestyles facilitated the continuation of care. Individual MSF clinical consultations, including routine testing, were discontinued; emphasis was placed on drug refills to reduce hospital waiting time; and treatments were dispensed for a longer period. These changes were fairly well accepted and understood. This Malawian teenager who came to renew her ARVs for three months, as opposed to two months before the pandemic, said, "I felt it was a good thing because I won't be coming here very often with all the things that are happening with Corona.
Teen clubs continued in Malawi. However, the suspension of meals in common, games, dancing and music that offered the possibility of living a "normal" and "enjoyable" life despite HIV was experienced as a loss. "It was hard because many children used to dance and play games like bawo, but now we were told to sit separately. [... MSF came to give advice and medicine," deplored one young participant.
In Uganda, a community-based ARV collection strategy was put in place for treatment refills during the period when patients were not allowed to go to the hospital, from April to July 2020. However, contact with people in DRC who cross the border to be followed by MSF in Arua has been difficult to maintain. Distribution of ARVs was partially done by a nurse in Aru, DRC, or by the few people who were able to travel to Uganda and bring back drugs to distribute to other patients in an impromptu community group.
Experiences sometimes different, but marked by difficulties
In addition to the abuse from authorities that it brought, strict confinement is often described in testimonies as having had a negative impact on life in general and the ability to manage one's HIV status at home. In Malawi, the fear of contracting Covid-19 and the difficulties of securing income and food were dominant. Especially since MSF had to suspend its social support activities during this period. The Covid-19 era is described as nthawi ya njala, literally a season of hunger, with the trade-off for people living with HIV being the difficulty of taking medication on an empty stomach, sometimes for days on end, which makes people feel nauseous and sometimes vomit.
This information should be considered in the development of new responses to future epidemics. While the response of health actors has allowed for the adaptation of ARV delivery modes and the maintenance of certain activities, the measures taken to protect people against the coronavirus have limited and sometimes even prevented access to care for people living with HIV. This raises the question of whether the measures taken to protect people from the coronavirus have been more deleterious than beneficial for people living with HIV and perhaps for other subgroups of the population.
(1) https://www.unaids.org/sites/default/files/media_asset/JC3032_AIDS_Data_book_2021_En.pdf